What is Sperm Banking & Why Should I Consider It?
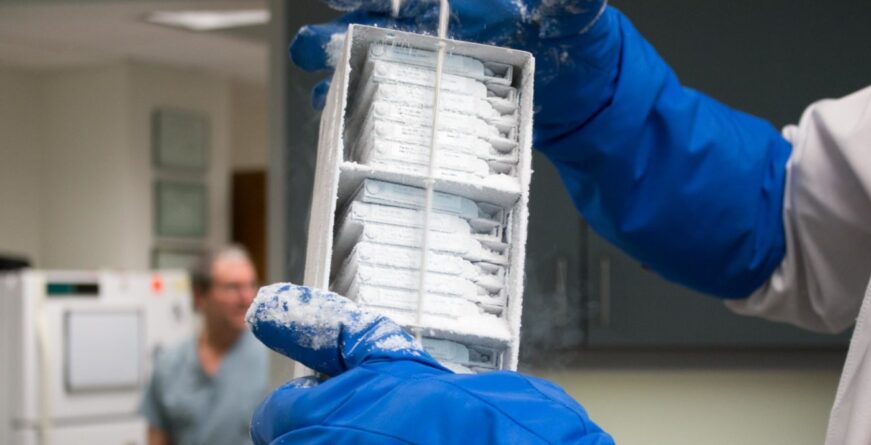
Whatever your reason for cryobanking, Maze Labs offers a full line of services to collect, freeze and store sperm. To ensure the future viability of your sperm, we first perform a thorough semen analysis prior to banking. A cryopreservative is added, and the specimen is divided into individual tubes, each labeled with multiple unique identifiers (showing it is yours).
After each specimen is frozen for 48 hours, we thaw a small sample and test it again to see how well it survived the freezing. This allows us to project how many moving sperm will be in each frozen vial; when it is eventually thawed when needed.
Why Banking at Maze is different:
In most cases we store some of your vials in two completely different facilities, adding extra protection. All tanks are monitored on a continuous 24/7 basis, and manually on a frequent basis.
Our bank is directed by Michael A. Werner, MD. who is a reproductive urologist. He reviews every specimen as it comes in. He will also work with your doctors when it comes time to use the specimen, in terms of which vials to release and how best to use them to achieve a pregnancy.
With modern reproductive techniques, fertilization has been possible with fewer and fewer sperm. The famous quote: "You only need one living sperm for each egg." is proving true. Even in cases where extremely few sperm are available to freeze, we have seen success.
It's important for Men to take action as early as possible and determine if Sperm Banking is right for them. A Man's fertility (at present or in the future) can be at risk for a variety of reasons. This includes cancer treatments, surgery, occupational hazards, general aging (the list continues). Other men are banking as directed donors (where the sperm will not be used with their sexually intimate partner). Fortunately, sperm can be frozen and stored, almost indefinitely, for future use. We will review many of the reasons to bank sperm below.
Contact us with questions or to schedule an appointment.
TOPICS COVERED
- What is cryopreservation/sperm banking?
- Who should consider banking their sperm?
- What is the process for banking sperm?
- Directed Donor Sperm
- Choosing a sperm bank
WHAT IS CRYOPRESERVATION/SPERM BANKING?
Cryopreservation is the process of freezing tissue. Sperm cryopreservation is the freezing of a man’s sperm for future use. A sperm cryobank is a facility that collects, stores, and freezes the sperm.
WHo should consider BANKING sperm?
Sperm banking is used for a variety of situations and the indications continue to rapidly expand. Below, are just some of the reasons why a man should seriously consider cryopreserving (banking) his sperm:
Cancer Treatments
Cancer treatments may include chemotherapy, radiation, or surgery. Radiation and chemotherapy can negatively affect a man’s sperm production- sometimes permanently destroying completely the ability to make new sperm. Some men do get recovery of sperm production at their original pre-treatment levels. Other men get return of sperm but at much lower levels than prior to treatment. (Surgeries for cancer in the pelvis may make it impossible for a man to ejaculate, and will be covered in a section below).
Chemotherapy and radiation can negatively affect the genetics of sperm being made at the time of treatment, and for up to 12 months afterwards; this leads to higher chance of abnormal offspring if these sperm lead to a conception. So sperm should be banked prior to treatment if fertility is desired in the next 12 months.
We are quite passionate about this work, and will often bank for adolescents and men who are already hospitalized, and need banking immediately. We work closely with various cancer centers, including Memorial Sloan Kettering.
Medications Causing Damage To Sperm
Certain medications are known to decrease sperm production and possibly increase the chance of abnormal offspring, both while you are taking them AND for the 6-12 months after you discontinue.
Here we have included a published table reviewing medications that can affect sperm production.
Men Receiving Testosterone Treatment (TRT)
In order for Men to make sperm, the testes need to be producing a very high concentration of testosterone. When Men go on TRT (take external testosterone), it will shut down a Man’s production of testosterone in his testes.
For this reason, t’s important for Men to consider banking sperm prior to treatment. Men who start on TRT feel dramatically better, so it can be difficult to stop treatment. Once a Man stops TRT, sperm production usually comes back, although this not guaranteed. (especially if pre-treatment sperm production was very low to begin with).
Men who have a low testosterone with clinical symptoms can also be treated with selective estrogen receptor modulators (SERM’s) or hCG to increase their production of testosterone, thereby preserving sperm production. However, Men will report feeling better using TRT as opposed to using select estrogen receptor modulators.
For Men who are interested testosterone replacement therapy (TRT) and are considering children in the future, we strongly recommend that men bank their sperm prior to starting treatment.
Trans Women Starting or on Hormonal Treatment
We have been banking the sperm of trans women for many years, and have developed an expertise and sensitivity in this area.
Hormonal treatments (that are essential for transitioning) almost always shut down sperm production. Ideally, women starting their medical transitions would bank sperm prior to starting therapy. This can be a stressful and emotional time, with a lot of decisions being made at once. Many trans women are not sure if they want children, or what the sex of their future partner will be can feel uncomfortable with their penis and ejaculation.
We feel strongly that banking sperm prior to that hormonal therapy is the best time. Of course, adolescent and preadolescent girls are transitioning at ever earlier ages, making collection of sperm pre-transition more difficult. Biologically, ejaculation begins around 13 ½ years old, with the range being from 12 ½ to 15 ½. It does seem like sperm production occurs during a similar time frame. However, in our experience, the ability to ejaculate may precede the appearance of sperm in the ejaculate.
We have found that with the encouragement of their parents, health professionals, and our lab, the vast majority of transitioning adolescent girls have been successful in producing specimens that can be frozen for possible later use.
Trans Women after Starting Hormonal Therapy
We are very proud in having pioneered the use of Extended Sperm Search and Microfreeze (ESSM) in the U.S. This technique can be used to find low levels of sperm in the ejaculate or in testicular tissue. We have found sperm in the ejaculate of a woman who had been on hormone therapy for 18 years. She had stopped hormonal therapy for 10 months prior.
Here is the link to the New York Times article describing this success. We have also found sperm in other women on long term hormonal therapy.
Even if you did not bank sperm prior to starting your transition, if your testes are still in place, there is a chance we can find sperm in your ejaculate or in the testes themselves.
Surgery
Scrotal Surgery:
Scrotal surgery can cause a decrease in testicular tissue producing sperm, most commonly from the removal of a testicle for cancer. Scrotal surgery can also cause a localized blockage of the epididymis (the first part of the tube carrying sperm from the testes). Of course a vasectomy will also stop you from ejaculating sperm.
Testicular Cancer:
Testicular cancer most commonly presents itself during adolescence, though it is rare. Sometimes these patients at the time of presentation, and even prior to surgery, have no sperm in the ejaculate (are azoospermic). It is possible that whatever made the testicle with the cancer more prone to cancer, can also be affecting the other testicle, in terms of sperm production. It could also be that the cancer in one testicle is inhibiting the production of the sperm in the other testicle. Sometimes, at the time of the removal of the testicle with cancer, some of the tissue may be removed and examined for sperm production. If sperm is found, it could then be frozen for later usage. This, of course, needs to be coordinated with the cancer surgeon and our laboratory prior to the surgery.
As testicular cancer occurs at a higher rate in the remaining testicle of a man who has had testicular cancer, all men with one remaining testicle should have their sperm banked.
Prostate Medications/Surgery/Procedures
Almost all men experience an enlargement of their prostates as they age. Treatment can involve medications or procedures/surgeries.
Medications:
The first line of treatment involves medications. Some of these medications can have a negative effect on sperm production or delivery.
For example, 5 alpha reductase inhibitors can shrink down the size of the prostate, but also decrease sperm production. Alpha blockers can cause a man’s ejaculation to be backwards into the bladder (retrograde ejaculation). Luckily, the effects of these medications are almost always reversible.
Prostate Procedures:
Currently, there are various procedures that can be performed on the prostate if medical treatment is not successful. Many of these procedures will either decrease (or stop) a man’s ability to ejaculate sperm. The mechanisms for this may be by blocking the ducts carrying the sperm, or by causing any sperm released during orgasm (technically emission) to be ejaculated backwards into the bladder (retrograde ejaculation).
Pelvic Surgery
Surgeries in a man’s pelvis and rectal area can damage the nerves needed for ejaculation. These include colon and rectal surgeries for cancer, or other non-cancer conditions (diverticulitis). Some men cannot ejaculate at all after surgery. Others have retrograde ejaculation, meaning the sperm go backwards into the bladder, and therefore are expelled with urination.
Ejaculatory Issues
In order for a man to achieve a conception sperm needs to be ejaculated out of his body, which normally occurs in several steps.
- The man has to put the fluid containing his sperm (ejaculate) in his urethra (emission).
- The man has to push it forward (antegrade) out of the tip of his penis (ejaculation).
Medical Conditions Affecting Ejaculation:
Certain medical conditions (and surgeries, as described above) can interfere with one or both of these steps, which require intact nerves. If a man is diagnosed with any of these conditions, and is noticing a progressive difficulty with routinely ejaculating normally, he should consider banking his sperm while he is able to. These conditions include:
- Diabetes
- Multiple Sclerosis
- Parkinson’s Disease
- Spinal cord stenosis or injury
Medications Affecting Ejaculation:
Certain medications can raise the threshold for ejaculation. The most common of these are the antianxiety/antidepressants including SSRI’s and SNRI’s. If ejaculation becomes erratic, sperm can be banked before treatment or even afterwards, whenever a man is able to ejaculate.
Pre-Vasectomy
A vasectomy should be considered a permanent method of sterilization. However, many men and/or their partners would like to keep the option of having children open for the future. Life circumstances do change (including a couple’s change of heart, man’s change in partner, tragedy). If sperm have been cryopreserved a pregnancy can be attempted without a surgical intervention to either reverse the vasectomy or harvest sperm. If the quality of the sperm is high enough, inseminations may be attempted with the frozen sperm. If not, IVF is the option of choice. Dr. Werner will work with you and your partner’s doctor if you decide to use the frozen sperm, on how to best utilize it.
Once deciding on a Vasectomy, many men and or couples are anxious to get it done quickly. Sperm banking can usually be done within a week.
Delayed Father-Hood
Paternal age has increased dramatically in the US in the past 40 years, and the trend seems to be continuing. The average age of paternity has gone from 27.4 to 30.9 years in the last 40 years.
In the 1970s, 4% of births were to fathers over the age of 40; today that number is 9%. Also in the 1970’s one in two hundred births were to fathers over 50; today this number has doubled.
Spermatogonial stem cells are the cells that divide and split, over a man’s lifetime, to produce sperm. Spontaneous mutations occur, and then generally become present in all of a man’s sperm. It can be estimated that the sperm produced from a 25-year old male has undergone ∼350 replications, while ∼750 replications would have taken place to sustain sperm production in a 45-year old male.
On average, approximately 1–2 additional mutations arise in the genome of a child per additional year in the age of the father. Thus, the number of mutations doubles with every additional 20 years of paternal age.
Unfortunately, increased paternal age has significant negative effects on conception rates, pregnancy outcomes, and the health of the offspring. The children of older men are at higher risk for genetic disorders, congenital abnormalities, neurodevelopment disorders, and malignancies. The American Society of Reproductive Medicine and the American Urological Association have issued joint male infertility guidelines, which include the suggestion that; “Clinicians should advise couples with advanced paternal age (≥40 years) that there is an increased risk of adverse health outcomes for their offspring (3).”
For men who know they want children and are delaying them for a number of reasons, it is reasonable for these men to consider banking their sperm. Frozen sperm are not dividing and thus are not subject to the copying errors inherent in ongoing sperm production, which increase over time.
The optimum time for this banking is subjective and unclear. However, if a man at or over 35 is projecting it will be five or more years before attempting a conception, it may be wise to bank for him to bank his sperm.
Low Levels of Sperm - Which May Go To Zero
Over time, all men’s sperm production deteriorates. Thus, many men with low numbers of motile sperm in their ejaculate will have their sperm production deteriorate over the course of months or years to the point where there is no longer sperm in the ejaculate.
Also, all men have variability in their semen analyses, even over a short period of time. If you have only very few sperm in your ejaculate, it is very possible that when you go to produce a fresh specimen for an in vitro fertilization (IVF) cycle, there will not be sperm present that day. Sperm frozen in advance can then be used as a backup.
Fortunately, all studies indicate that fertility rates are identical for fresh versus frozen sperm, as long as moving (motile) sperm are found. Thus, all men with very low numbers should bank both for longer term and shorter term use.
Men with very low numbers can have their sperm processed by our lab, using Extended Sperm Search and Micro-freeze (ESSM). We can find and freeze sperm in situations where other labs can’t.
This processing procedure allows us often to find sperm not found on a traditional semen analysis. It also freezes the sperm on specialized dishes in small volumes of fluid. This makes them easy to find when needed. The freezing technique is also different from that used on other specimens, giving a very high rate of post thaw live sperm survival.
Prior to Advanced Reproductive Procedures
More and more couples are requiring advanced reproductive techniques (ART) in order to achieve a conception. These include intrauterine inseminations (IUI’s) and in vitro fertilization (IVF). It is common to bank sperm prior to these procedures for several reasons. Some men cannot produce a specimen the day of the planned procedure, due to pressure and anxiety. Others have unpredictable and low sperm production, and there may not be enough sperm in the ejaculate the day of the procedure.
We bank the sperm of many straight and gay couples and individuals planning to use a surrogate to carry their baby. In these cases, many states require the sperm be banked in advance, and the men tested at the time of banking and six months later for STI’s. In other words, their sperm must be treated as those of designated donors, since the embryos made with their sperm will be placed in the uterus of a woman who is not their sexually intimate partner. (Link to designated donors)
Occupational Hazards
Certain occupations expose men to increased heat or toxins, which can decrease sperm production. These include:
- Industrial Chemicals
- Pesticides, heavy metals, painting materials
- Radiation Exposure-including X rays
- Increased Testicular Temperature: The testes need to stay below body temperature, which is why they are located outside a man’s body. Frequent exposure to heat can cause a decrease in sperm production. This includes:
- –Truck driving for long periods of time
- –Professional Cooking (bakers, chefs, pizza makers)
Surgical Sperm Retrieval (SSR)
Sometimes sperm need to be procedurally procured (Surgical Sperm Retrieval or SSR) from a man because he has an obstruction or very low sperm numbers. Sperm may be harvested from the testicle, epididymis, or vas deferens. These sperm always need to be combined with an in-vitro fertilization procedure, and the sperm injected directly into the egg; this is because they are low in number, and often have limited movement (they are alive, but do not have enough forward movement to make their way naturally through a woman’s reproductive tract.)
Sperm are sometimes procured in advance and frozen. Other times the sperm are procured the day of egg retrieval and used fresh. In these situations there are often more sperm procured than needed for that one cycle, and these can often be cryopreserved and used in the future, saving the man an additional procurement procedure. (We often will both search for sperm in the surgically procured specimen as well as freeze the extra ones using ESSM)
Klinefelter’s Syndrome
Men with Klinefelter’s Syndrome (who have one or more extra X chromosomes) may have either low numbers of sperm in their ejaculate or none. Many of these men will never have sperm production. However, many do, but if so the production peaks quite early, and then rapidly decreases after adolescence.
If sperm are ever found in the ejaculate, they should be immediately cryopreserved. In our laboratory, many of these men undergo Extended Sperm Search and Microfreeze (ESSM), which allows us to find and cryopreserve very low levels of sperm.
Can I bank sperm if I have Hepatitis?
Men with infectious diseases can bank their sperm at Maze Cryobank. Men with known infectious diseases immediately have their specimens placed in a special tank, reserved only for specimens of men with that disease. We have two separate tanks, one each for specimens of men with Hepatitis B and Hepatitis C. These specimens are NEVER placed in tanks with specimens of men without this particular infection. However, for the men with hepatitis we offer a banking option.
WHAT IS THE PROCESS FOR BANKING SPERM?
Sperm banking is, in most cases, a simple and straightforward process. It is not time consuming or "appointment intensive." Although the process differs slightly between cryobanks, the basic procedure is the same:
- An appointment is set with the laboratory to meet with a lab representative, review your case history and medical background, and fill out necessary paperwork, and produce your first specimen.
- Many labs require an initial test freeze of the sperm before actually conducting the banking and they may require that you return for a second appointment. However, there is no advantage to this. In our lab, a full analysis is done on the first specimen (which requires very little of the specimen). If it is adequate for cryopreservation, it is then processed and frozen. It is important not to waste this specimen, as often there is a small window of time to bank a man’s sperm, before treatment begins. This leaves only enough time for a man to produce and bank a limited number of specimens.
- You may be given a choice of producing a specimen at home or at the lab site. If you choose to collect at a laboratory you will be given a private room. Visual material may also be made available to you. If you choose to collect at home you will be given clear and exact instructions. Ideally, if you produce the specimen outside of the laboratory, it would arrive at the lab within 60 minutes. However, though this is ideal, many of the sperm will still be alive hours after production. Do not assume that if your specimen does not reach the laboratory within an hour it is useless. Also, do not assume that just because you are hospitalized more than an hour away from the bank, that you will be unable to cryopreserve your sperm. It is important to ask all of these questions when arranging your appointment.
How is sperm actually frozen?
Frozen sperm must be stored in extremely cold temperatures (-196 F), but in order to insure that the fewest possible sperm are damaged, the freezing must be gradual. Generally, the following procedure is followed:
- If the sperm hasn’t been previously tested, a comprehensive semen analysis should be performed on the first specimen in order to give you a complete picture of your sperm quantity and quality. Make sure that your sperm bank conducts a thorough semen analysis before banking. This will give you significant information on the quality of the sperm, which helps determine how it can be used when you desire to initiate a conception.
- Each subsequent specimen is analyzed prior to freezing to assess concentration, motility, forward progression, semen quality, and total number of moving sperm.
- Immediately after the specimen is analyzed, and prior to freezing, a special fluid (a cryoprotectant) is added to aid the freezing process. This helps the sperm survive the freezing and the subsequent thawing process, which is performed when they are ready to be used or tested.
- The combined fluid (semen plus cryoprotectant) is then divided into portions and placed in separate vials. Each vial holds up to 2 cc’s (a teaspoon is 5 cc’s). A small amount of the combination fluid (specimen and cryoprotectant) is placed in a separate vial (test or T- vial). This is usually about 0.2 cc’s or less.
- The test tubes are gradually frozen. After 30-60 minutes they are transferred into liquid nitrogen tanks for permanent frozen storage.
- After a minimum of 24 hours has elapsed from the time of the initial freezing, the test vial is thawed and tested again. This is to ascertain from each test thaw specimen how well the sperm survived the freezing and subsequent thawing, in terms of number of sperm, percentage moving, and quality of the movement. From these results, we will be able to project with reasonable accuracy the quantity and quality of moving sperm that will be found in each of the storage vials when they are thawed for use in the future.
How is Sperm Stored?
Vial Labeling:
Each vial is assigned a unique accession number, and is labeled with six pieces of information:
- Patient’s full name
- Banking Date
- MAZE Laboratories
- Accession number
- Patient’s date of birth
- Last four digits of the patient’s social security number
Vial Storage:
The vials are placed in temporary storage until you are finished banking, and all of your blood work comes back and shows that you are negative for infectious diseases. Then they are placed into permanent storage, in large tanks. Within the tanks, there are individual racks, with numbered slots. Each vial goes into a unique slot, the identity of which is recorded and then saved in multiple locations, so it can be easily and accurately found.
- One tank versus two tanks. At Maze, we store almost all patients’ specimens in two different tanks, in two different locations. This is added protection, in case there was ever a problem with a tank. Though the chances of this happening are extremely low, we believe it’s worth taking the added precaution of a second tank.
- How are the tanks monitored?Each tank has its own continuous temperature monitoring system. If the temperature increases even slightly, to a few points above -196 F, then the alarm goes off. (The sperm are still safe at temperatures way above this.) The alarm is then sent through an automatic calling system to alert our staff, one of whom is on call at all times, who will rectify the situation. The system has a large back up battery in our offices, and then a backup generator connected to this.
It is important that you ask a sperm bank how their tanks are monitored prior to considering using their services. We have been amazed that some banks do not have continuous monitoring, and no alarm system whatsoever. They rely entirely on periodic checks of the tanks.
How will my specimens ultimately be used?
In order to use your frozen sperm, the recipient will need to work with an ob/gyn, usually a specialist in female infertility, even if she has no fertility issues.
There are two main methods used, intrauterine inseminations (IUI’s), and in vitro fertilization (IVF).
Intrauterine Inseminations (IUI’s):
For an IUI (which is also done frequently for couples with infertility using fresh sperm) the frozen sperm are thawed and then processed or washed prior to being placed in the woman’s uterus with a small catheter.
The sperm must be processed because many of the components of semen and the cryopreservative should not be placed directly in the uterus. (When a couple has intercourse, the sperm push their way through the cervical mucus, and leave behind the rest of the fluid naturally.)
The sperm then need to make their way up the woman’s fallopian tubes, where fertilization usually takes place. (In fact, during the processing, the sperm are placed in a nurturing solution which mimics the fluid found naturally in a woman’s fallopian tubes, called HTF, or Human Tubal Factor.) Many sperm bind to the egg’s outer membrane, and then finally one breaks through to fertilize the egg.
In order for IUI’s to have a reasonable chance of success, the specimen needs to have many moving sperm, as so many are lost as they make their way up the tubes and so many sperm need to bind to each egg prior to fertilization.
Thus, IUI’s are not considered a reasonable option, unless the total number of moving sperm in the specimen, after thawing, is between 5 and 10 million. Several frozen vials can be combined in order to reach the 10 million number. However, if it is projected that your vials, once thawed, will on average contain fewer than 2-3 million moving sperm, per vial, you probably should not try to use them for IUI’s.
IUI’s have a lower success rate than IVF, and thus you would have to assume that it will take 2-3 cycles on average to have a reasonable chance of achieving a conception. If each of your vials yields more than 10 million moving sperm, a single vial could be used for each IUI. If each of your vials yields 3-9 million, you would probably use more than one vial per IUI.
Thus, the men whose numbers are in this intermediate range, 3-9 million moving sperm post thaw, will need to bank the most vials, if they want to try to achieve a conception with IUI’s.
The advantages of IUI’s are that they are less invasive for the woman and less expensive. This is why they are preferred to IVF in many cases, if it is a reasonable option based on both the quality and quantity of the sperm, and on female factors.
In Vitro Fertilization (IVF):
With IVF, the woman is given hormones to make her produce many eggs. These eggs are then harvested, by placing a needle that goes through the vagina and into each follicle containing an egg. (This is done under general anesthesia, but most women have very little discomfort afterwards.)
Originally, each egg was placed in its own dish, and the sperm put into the dish, to try to achieve fertilization. This is called conventional IVF, and each egg needs about one million moving sperm to have a reasonable chance for fertilization to take place.
However, in most cases involving frozen sperm, the specimen is thawed and an individual moving sperm is taken and injected directly into an egg, which is called ICSI (Intracytoplasmic sperm injections).
For ICSI to be a viable option, a man only needs one moving sperm per egg to be available. Thus, with the advent of ICSI, it became worthwhile for men with extremely low counts to bank their sperm, because they then had reasonable chances of achieving a conception.
How many specimens should I bank?
To decide how many specimens to bank, it’s important to understand how they will be used, when and if you need them. One of the most important advantages of Maze Cryobank is that its medical director, Michael Werner, MD, is a specialist in male infertility.
He will be reviewing the results of your bankings as they are happening, and helping you decide how many specimens make sense in your particular case. Active decisions must also be made, in real time, as a particular specimen is being prepared, in terms of how many vials are made from it, and what volume they should be. This will depend on several factors, including the volume of the ejaculate, the quality and quantity of the sperm, and how many bankings you will have time for prior to beginning treatment.
The number of specimens you should bank will depend on several variables
1. How Many Sperm You Have in the Post-Thaw Specimen
As can be seen above, if you have enough sperm in the post-thaw specimens to do IUI’s, you will want to have enough vials to do several IUI’s and have some vials left over so that you can do some IVF’s in case the IUI’s are not successful.
Thus, men with total post thaw motile counts of greater than 10 million sperm/vial, will want to have on, average, 12-15 vials.
The men with total post thaw motile counts between 3-9 million/vial, will probably want almost 20 vials, so that some can be pooled to get up to 10 million for each IUI attempt. Some vials should be reserved for IVF if the IUI’s are not successful.
Most men with post thaw motile counts of less than 2 million will probably only need 10 vials. Each vial can be used for an IVF, and there are very few situations where more than 10 IVF’s could be reasonably anticipated.
Some men have extremely low numbers of sperm in the ejaculate, and some, if not all, of their specimens would be anticipated to have very low numbers of moving sperm post-thaw. In these cases, sometimes many specimens are banked to make it more likely that any moving sperm will be found post-thaw. In other words, sometimes multiple vials may be needed even for an IVF, in order to find enough moving sperm to have one for each egg. However, in these cases we now usually recommend Extended Sperm Search and Microfreeze (ESSM).
2. How Much Time You Have to Bank Before Beginning Treatment
Some men are banking sperm because they are very ill and treatment is imminent. They may only have time for one or two specimens before treatment is started. We often receive specimens from hospitalized patients who are too sick to be discharged from the hospital prior to treatment.
We try our best to make sure that each man gets 10 vials. We divide them up to give us more options in terms of using them (see above.)
3. Who Your Partner is Going to Be
Many men bank who are already partnered with a particular woman. Some may even already have children, but know they want more, or want to leave the option open. If possible, they should bank enough sperm for IUI’s and then IVF if necessary, as described above.
Many heterosexual men bank, without knowing who their partner will be. They want to leave the option of having enough sperm for IUI’s and then IVF if necessary.
Many gay men bank their sperm in anticipation of becoming fathers. Most will need to use a donor egg and a gestational surrogate. In these cases, IVF must be used, and 10 vials are enough. If they may be in a situation where the woman carrying the child is also supplying the eggs, then IUI’s are an option, and more vials may be needed.
How do I get my sperm from the bank?
Once you are ready to initiate a conception, you will need to begin working with an ob/gyn. If IUI’s are being considered, some general ob/gyn’s are comfortable with this process and will stay involved. In most cases, a specialist in female infertility, called a reproductive endocrinologist (RE) will be involved.
The female infertility specialist will want to know the quality and quantity of the vials you have stored, as well as the woman/women who will be supplying the eggs and carrying the child (which may be the same woman or two different women), prior to deciding how to best use them to achieve a conception.
Often, Dr. Werner, an expert in male infertility and andrology, will work with you and your female infertility specialists to determine the best course of action.
Once the number of vials to be used in a particular cycle has been determined, it will be your responsibility to contact our laboratory to release the specimens. You will also need to contact your RE’s lab so they are prepared to receive them. We will help make this easy for you. You then have the option of renting a small portable tank, and transporting the specimen yourself. Or you can have us ship the specimen in a larger tank for you.
How long should I store my sperm?
Pregnancies have been initiated with sperm that have been frozen (cryopreserved) for up to 21 years. However, there is no indication that sperm cryobanked for even longer are not capable of initiating a conception. Thus, it is important to bank your sperm for any of the indications listed above, no matter how long you think it may be before you would use them, or even if you are not sure you ever plan to have a family.
You should bank for as long as you think you may need the sperm. You should hope for the best outcome in terms of sperm production post treatment, and plan for the worst.
If you are young, and not anticipating trying to initiate a conception for a while, then you should bank for a longer time, 10- 20 years. (Always remember that you can contract for additional time once your contract comes close to expiring.)
If you are in a relationship, you should try to anticipate the farthest out you would like children for, and store for this period of time.
In some situations, there is only a minimal chance that a drug or surgery will cause infertility. In this case, you may want to bank for only a year or two. Then, if post treatment testing shows good return of sperm and/or ejaculation, the frozen sperm can be destroyed.
How long should I wait after treatment to check my sperm production?
Different courses of treatment have higher or lower probabilities of causing temporary or permanent damage to the sperm producing cells. Many men whose sperm counts go down dramatically during and right after treatment will have return of sperm production over time.
Sometimes, mens’ post treatment counts are even better after a period of time than the ones they banked prior to treatment. This is because their original condition (i.e. cancer or other medical conditions) can itself suppress their sperm production. Once the condition has been treated, the sperm production may improve on its own. This may be true even of men with testicular cancer. The cancer in this testicle may be suppressing production of sperm in the opposite testicle. Once the cancer is removed, and if your body recovers from treatment, your specimens may be better after the orchiectomy than prior to it. Unfortunately, they may also be worse, if there is damage to the remaining testicle from treatment, or if the remaining testicle never had good sperm production to begin with.
In general, we would suggest waiting at least a year after treatment to check your semen analysis. If the one year post treatment semen analysis is worse than the banked specimens, we generally suggest you keep the banked specimens and re-check the semen analysis in another year.
Some men may go down to zero for prolonged periods of time, and then gradually have some sperm production. The longer you are out from treatment, without the return of sperm, the less likely it will return.
DirecTED DONOR SPERM
Sometimes, the sperm of a man who is not a woman’s sexual partner is wanted to initiate a pregnancy. In this case, the conception will not be achieved through intercourse. However, legally, a physician cannot be involved in the transfer of fresh sperm from a man who is not the sexually intimate partner of a woman.
In New York State, the license and process for banking directed donor sperm is the same as it is for anonymous sperm donation. Maze Cryobank has this license, and does sperm banking for directed donors on a regular basis. Learn more about our Directed Donor services.
CONSIDERATIONS WHEN CHOOSING A SPERM BANK
There are numerous considerations that come into play in choosing a sperm bank. These include:
- Safety of your specimens — separated into different tanks, each with constant monitoring
- Clinical expertise of director — both from a scientific point of view, and a clinical point of view
- Location and convenience
Specimen Safety
Specimens stored in two different tanks:
Almost all of our patients bank multiple vials. For virtually all of the patients, some of your vials will be kept in a tank in our Westchester office, and the rest in our NYC office. Though tank malfunctions are extremely rare, having two tanks builds in an extra safety net in case of an unforeseen disaster, either to a particular tank or a particular location.
Tank Monitoring:
It is highly recommended that the status of each and every tank be monitored continuously. Some labs have no tank monitoring, except periodic manual checks.
At Maze, each tank is continuously monitored 24/7/365. If the temperature or level falls, an alarm goes off, which then phones our lab technician or physician on call. The alarm system has a battery backup, and a generator back up as well.
We would suggest you ask any sperm bank you are thinking of using how they monitor their tanks.
Clinical Expertise
Clinical Expertise:
Michael A. Werner, MD, the owner and Medical Director of Maze, is a board certified urologist, with a fellowship in male infertility, andrology, and male sexual dysfunction. He supervises the entire process of sperm banking, including helping decide how many vials to divide a particular specimen into, and how many times a man should bank. He works closely with the female infertility specialist when it comes time to use the vials. This comes from his knowledge base in the field of fertility as well as in his scientific knowledge of sperm production, analysis, processing, and freezing. His knowledge also often comes into play in situations where men have problems producing specimens.
Location & Convenience
Location:
Maze Labs has two locations. One is in Westchester County, (right by the intersections of I-95, I-287, and the Hutchinson River Parkway.) The second is at 633 3rd Avenue (between East 40th and 41st Streets, three blocks from Grand Central Station in New York City).
Hours:
We have early morning and evening hours Monday-Friday. It is often important to get several specimens banked quickly before treatment begins. We go out of our way to make sure you can do this.
